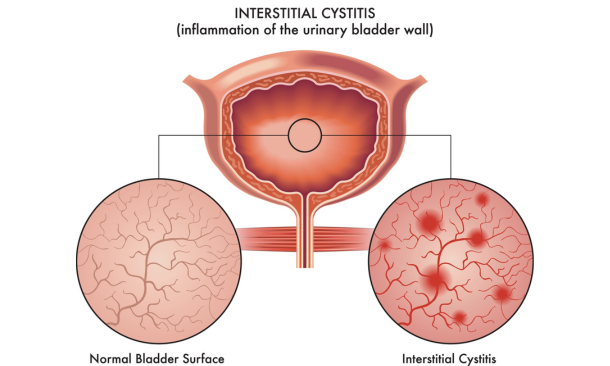
Interstitial cystitis treatment requires a multifaceted approach tailored to your unique needs. Interstitial cystitis (IC), often referred to as painful bladder syndrome, is a chronic condition affecting the bladder. It’s characterized by intense pelvic pain, urinary frequency, urge incontinence, and pain with intercourse.
IC is a debilitating condition that affects millions of people worldwide, predominantly women. At Propel Physiotherapy, our team of pelvic physiotherapists has seen the profound impact this condition has on every aspect of our clients’ lives.
Despite its prevalence, IC remains widely misunderstood, leading to misdiagnoses and inadequate treatment plans for those suffering with this condition. In this blog, we delve into the complexities of interstitial cystitis, exploring its symptoms, potential causes, and available interstitial cystitis treatment.
Table of Contents
- What is Interstitial Cystitis?
- Interstitial Cystitis Causes and Triggers
- Interstitial Cystitis Treatment
- Living Well with Interstitial Cystitis
- Interstitial Cystitis Treatment Conclusion
What is Interstitial Cystitis?
Interstitial cystitis is when an inflamed and irritated bladder wall can lead to scarring and stiffening of the bladder. Its symptoms can vary widely among individuals, making diagnosis challenging.
Some common symptoms include:
- Pelvic Pain: Persistent, often severe pain in the pelvic region is a hallmark sign of IC. This pain may fluctuate in intensity and may worsen as the bladder fills.
- Urinary Urgency and Frequency: Individuals with IC often experience a frequent urge to urinate, even when the bladder contains only small amounts of urine. This urgency can disrupt daily activities and sleep patterns.
- Painful Intercourse: Many IC sufferers experience pain during sexual intercourse, further impacting their quality of life.
- Nocturia: Frequent nighttime urination is common among IC patients, contributing to sleep disturbances and fatigue.
You may also enjoy reading: Urinary Incontinence Treatment
Interstitial Cystitis Causes and Triggers
The exact cause of interstitial cystitis remains unknown, which complicates treatment efforts. However, several factors may contribute to its development:
- Bladder Lining Defects: Some researchers believe that abnormalities in the bladder lining may play a role in the development of IC. These defects could compromise the bladder’s protective barrier, leading to inflammation and pain.
- Autoimmune Response: There’s evidence to suggest that IC may involve an autoimmune component, where the body’s immune system mistakenly attacks the bladder tissues, triggering inflammation and discomfort.
- Neurological Factors: Dysfunction in the nervous system may also contribute to IC symptoms. Nerve signals related to bladder control and sensation may be disrupted, leading to abnormal bladder function.
- Triggers: Certain foods, beverages, and activities can exacerbate IC symptoms in some individuals. Common triggers include spicy foods, caffeine, alcohol, stress, and hormonal fluctuations.
You may also enjoy reading: Pelvic Floor Exercises for Incontinence
Interstitial Cystitis Treatment
I can empathize with my clients’ frustration at the unpredictable and often debilitating nature of this condition. Finding help often becomes discouraging as managing IC requires a multifaceted approach tailored to your unique needs.
While there is no cure for IC, having someone you can talk to about your condition who understands how best to guide you through symptom-management techniques plays an invaluable role in improving quality of life.
Pelvic floor physiotherapy can be effective in relieving pelvic pain and improving bladder function through targeted exercises and relaxation techniques. Here is how physiotherapists trained in pelvic floor physiotherapy can aid in the treatment of IC:
- Pelvic Floor Muscle Therapy: Teaching exercises to strengthen and relax the pelvic floor muscles. Tight or tense pelvic floor muscles can contribute to bladder dysfunction and exacerbate IC symptoms. Learning to relax these muscles can help reduce pain and urinary urgency.
- Biofeedback: Biofeedback techniques may be used to help patients gain awareness and control over their pelvic floor muscles. By providing visual or auditory cues, biofeedback helps individuals learn proper muscle coordination and relaxation techniques, which can aid in managing IC symptoms.
- Manual Therapy: Manual techniques such as soft tissue massage or myofascial release can help relieve tension and trigger points in the pelvic floor muscles. This can reduce pain and discomfort associated with IC.
- Bladder Retraining: Assist with bladder retraining programs to help individuals gradually increase the intervals between urination and reduce urinary urgency.
- Education and Lifestyle Modifications: Provide education on IC triggers and lifestyle modifications that may help alleviate symptoms. This can include dietary changes, stress management techniques, and strategies for better bladder health.
- Modalities: Certain modalities such as heat therapy or transcutaneous electrical nerve stimulation (TENS) may provide temporary relief from IC symptoms by reducing pain and promoting muscle relaxation
You may also enjoy reading: Diastatis Recti Physiotherapy
Living Well with Interstitial Cystitis
Living with IC can be challenging, but with the right support and management strategies, individuals can lead fulfilling lives. Support groups, online communities, counseling services, and specialized healthcare professionals can provide invaluable support and guidance for coping with IC’s impact on daily life.
You may also enjoy reading: 5 Important Roles Pelvic Floor Muscles Play
Interstitial Cystitis Treatment Conclusion
Interstitial cystitis is a complex condition that profoundly affects individuals’ physical and emotional well-being. By raising awareness, promoting research, and offering comprehensive care, we can improve outcomes and enhance the quality of life for IC patients.
If you or someone you know experiences symptoms suggestive of IC, don’t hesitate to seek evaluation and support from healthcare professionals specializing in managing this condition.
At Propel Physiotherapy, we’re committed to providing holistic care and support for individuals living with IC. Contact us today to learn more about how we can help you on your journey to relief.
Written by